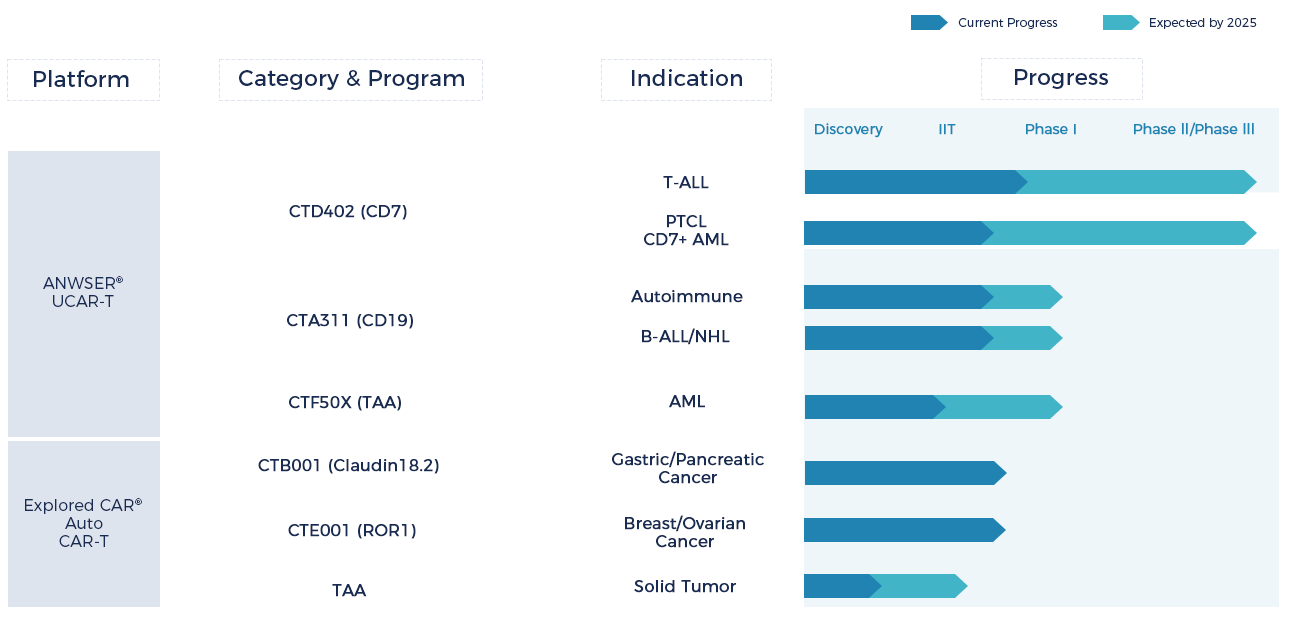
Pipeline
Our pipelines focus on oncology and autoimmune diseases
Technology Platforms
Our platforms – featuring ANSWER® CAR, Explored CAR® and RVVpacReady®
ANSWER® 2nd Gen UCAR-T
Onco & Non-onco
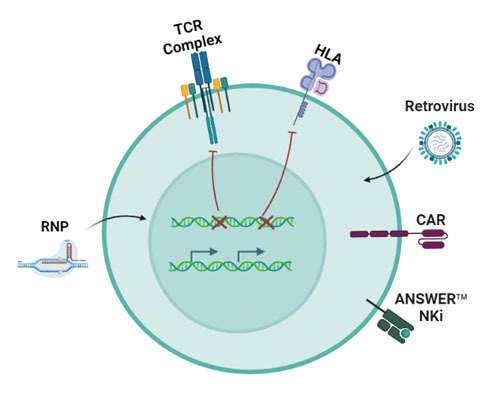
NK inhibition strategy: KO TCR, HLA and overexpress NK inhibitory molecule
Explored CAR®
Solid Tumor
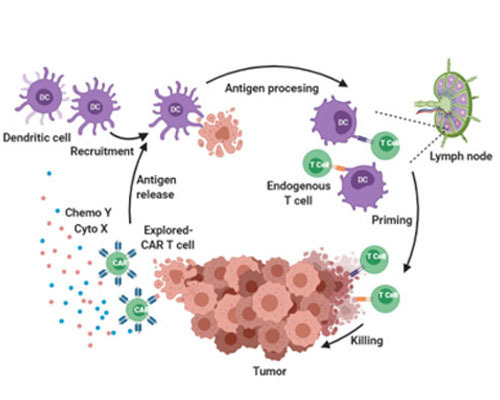
Solid tumor Armored CAR-T strategy: Secrete payload cytokine and chemokine to evoke in situ immune response
RVVpacReady®
Viral Vector
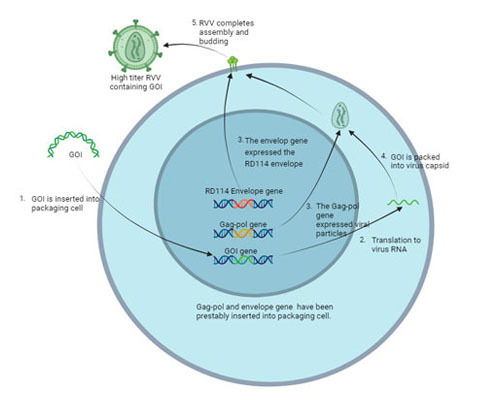
Higher harvest titer and transduction efficiency with lower COGS and impurities
Publications
Recently published articles
Chimeric antigen receptor (CAR)-T cell therapies for T-cell malignancies face significant challenges, including cannibalism among CAR-T cells and product contamination from cell explosion. Allogeneic CAR-T cells generated from healthy donor T cells can provide ready-to-use, blast-free therapeutic products, but their application may be complicated by graft-versus-host disease (GvHD) and host rejection. Here, we developed CD7-targeting CAR-T cells (RD13-01) from healthy donors that were genetically modified to resist cannibalism, GvHD, and allorejection and to enhance antitumor function . A phase I clinical trial (NCT04538599) enrolled 12 patients (11 with T-cell leukemia/lymphoma and 1 with CD7-expressing acute myeloid leukemia). All patients achieved the prespecified endpoint, and 11 patients were evaluated for efficacy. No dose-limiting toxicities, GvHD, immune effector cell-related neurotoxicity, or severe cytokine release syndrome (≥Grade 3) were observed. After 28 days of infusion, 81.8% (9/11) of patients experienced objective response, with a complete response rate of 63.6% (7/11, including AML patients). Three responding patients received allogeneic hematopoietic stem cell transplantation. At a median follow-up of 10.5 months, 4 patients remained in complete response. Reactivation of cytomegalovirus (CMV) and/or Epstein-Barr virus (EBV) was observed in several patients, one of whom died from EBV-related diffuse large B-cell lymphoma (DLBCL). Expansion of CD7-negative normal T cells was detected after infusion. In summary, we present the first report of a phase I clinical trial using healthy donor-derived CD7-targeting allogeneic CAR-T cells to treat CD7+ hematological malignancies. Our results demonstrate the encouraging safety and efficacy of RD13-01 allogeneic CAR-T cells for the treatment of CD7+ tumors.
Purpose: Autologous chimeric antigen receptor T (CAR-T) cell therapy is an effective treatment for relapsed/refractory acute lymphocytic leukemia (r/r ALL). However, the use of autologous CAR-T cells with certain characteristics may delay the availability of therapy. Another problem caused by antigen escape after relapsed single-target CAR-T treatment. Therefore, we aim to develop CRISPR-edited universal off-the-shelf CD19/CD22 dual-targeting CAR-T cells as a novel therapy for the treatment of refractory ALL. PATIENTS AND METHODS: In this open-label, dose-escalation phase I study, a universal CD19/CD22-targeted CAR-T cell (CTA101) CRISPR/Cas9 disrupted the TRAC region and the CD52 gene to avoid host immune-mediated rejection was injected. /r All in the patient's body. Safety, efficacy, and CTA101 cell kinetics were assessed. Results: CRISPR/Cas9 technology mediates efficient, high-fidelity gene editing and production of universal CAR-T
Background: T-cell acute lymphoblastic leukemia (T-ALL) and T-cell lymphoblastic lymphoma (T-LBL) are highly aggressive T-lineage malignancies characterized by an infiltration of immature T cells in the bone marrow (BM) and peripheral blood (PB) or extramedullary organ involvements. Effective treatments were elusive, and the long-term survival of patients with refractory/relapsed (R/R) T-ALL/LBL remains poor despite allogeneic hematopoietic stem cell transplantation (allo-HSCT). CAR-T therapies for T-cell malignancies remain underdeveloped due to the shared antigenicity between normal and malignant T cells. CD7 is highly expressed on the surface of T-ALL/LBL T cells and is considered a viable CAR-T therapeutic target. However, CD7-targeting immunotherapies may be compromised by T-cell fratricide and extermination. And one of the biggest challenges with autologous CAR-T cell therapy is to isolate a sufficient number of healthy T cells from malignant T cells. Thus, clustered regularly interspaced short palindromic repeats (CRISPR)/CRISPR9-associated protein 9 (Cas9)-mediated gene ablation has been used to produce universal CD7-targeted CAR T cells (UCD7-CAR) from suitable healthy donors that no longer express CD7 and TCR. In vitro killing tests, animal tests, and phase 1 clinical trials have preliminarily verified the efficacy and safety of universal CD7 CAR-T cells. Here we investigated the safety and efficacy of the universal CD7 CAR-T therapy in phase 2 clinical trial(NCT05454241) for pediatric R/R T-ALL/LBL patients.
Background: T-cell acute lymphoblastic leukemia (T-ALL) and T-cell lymphoblastic lymphoma (T-LBL) are highly aggressive T-lineage malignancies characterized by an infiltration of immature T cells in the bone marrow (BM) and peripheral blood (PB) or extramedullary organ involvements. Effective treatments were elusive, and the long-term survival of patients with refractory/relapsed (R/R) T-ALL/LBL remains poor despite allogeneic hematopoietic stem cell transplantation (allo-HSCT). CAR-T therapies for T-cell malignancies remain underdeveloped due to the shared antigenicity between normal and malignant T cells. CD7 is highly expressed on the surface of T-ALL/LBL T cells and is considered a viable CAR-T therapeutic target. However, CD7-targeting immunotherapies may be compromised by T-cell fratricide and extermination. And one of the biggest challenges with autologous CAR-T cell therapy is to isolate a sufficient number of healthy T cells from malignant T cells. Thus, clustered regularly interspaced short palindromic repeats (CRISPR)/CRISPR9-associated protein 9 (Cas9)-mediated gene ablation has been used to produce universal CD7-targeted CAR T cells (UCD7-CAR) from suitable healthy donors that no longer express CD7 and TCR. In vitro killing tests, animal tests, and phase 1 clinical trials have preliminarily verified the efficacy and safety of universal CD7 CAR-T cells. Here we investigated the safety and efficacy of the universal CD7 CAR-T therapy in phase 2 clinical trial(NCT05454241) for pediatric R/R T-ALL/LBL patients.
Although autologous CAR-T therapy targeting CD19+ B-cell has proven efficacy in hematological malignancies. The challenges such as undesirable waiting time, possible manufacturing failures and high cost, remain to be solved. In addition, antigen-loss/downregulation leads to treatment failure after single-target CAR-T therapy. To tackle these issues, we developed a universal CD19/CD22-targeting CAR-T cell with the TRAC region and CD52 gene disrupted using CRISPR/Cas9 technology. Pre-clinical data demonstrated the safety of CRISPR gene editing and the anti-leukemia ability of CTA101.
Contact Us





